It occurs at least every other week in my own clinical experience. A patient has experienced an ischemic stroke, and after a workup that fails to show significant atherosclerosis (“hardening of the arteries,” “plaque build-up”) in the arteries leading to the part of the brain injured by the stroke, and without obvious risk factors that could have resulted in stroke, an echocardiogram identifies the presence of a patent foramen ovale (PFO). Often patients are told a PFO is a “hole in the heart,” allowing clots to reach the brain that would otherwise end up in the lungs as their final destination. I see in their notes: “Stroke caused by PFO.” Some patients arrive to the appointment, already having determined they want their PFOs closed, and others have already concluded just the opposite – no “heart surgery.” The majority feel lost and are seeking answers. What is a PFO, and what is the significance of it?
The purpose of this post is outlined in the title – to remove some of the mystery from the PFO, although its potential effects and clinical associations with it are, indeed, still mysterious.

In the fetal heart prior to birth, blood enters the right atrium (A). Some of this blood circulates through an opening called the foramen ovale (yellow arrow in image), and into the left atrium (B), bypassing the lungs. When the foramen ovale fails to close, it becomes known as a patent foramen ovale, or PFO. Image source: http://vhlab.umn.edu
A foramen ovale (“FO” – if you will) is a very normal part of a fetus’s heart. When we are fetuses, prior to taking our first breaths as our developing lungs remain collapsed, blood bypasses the lungs and receives oxygen from the placenta. As blood enters the right atrium of the heart, it can bypass the lungs by traveling through the foramen ovale, an opening connecting the right and left sides of the heart. After reaching the left side of the heart, blood can then proceed to travel through the left atrium, then the left ventricle, and finally exiting the heart through the aorta. Other features of fetal circulation exist to enable blood to more efficiently reach the placenta, such as the ductus arteriosis, which allows blood to stream from the pulmonary artery directly to the aorta rather than first having to visit the lungs.
A “FO” becomes a “PFO” (“patent” merely means “open”) when that opening between the right and left sides of the heart fails to close completely.
A PFO is not a congenital heart defect. This is an important piece of information for stroke patients found to have a PFO to understand. Many of them arrive at their appointment, believing there is something wrong with their hearts. It is a normal part of fetal circulation to have a foramen ovale.
PFOs are common. Population studies indicate that 20-25% of people have a PFO, and the overwhelming majority of them will never experience a stroke related to this opening between the right and left atria in the heart. However, when younger people with cryptogenic ischemic stroke (stroke without an identifiable cause) are screened for PFOs, one is found in about 40% of patients being evaluated. This finding has been confirmed in multiple studies.
Screening for PFOs. Typically, a PFO is identified on an echocardiogram, which is an ultrasound study of the heart. Sometimes if there is significant blood flow through the PFO this can be identified on a standard echocardiogram. However, much of the time this is found after a bubble study, or agitated saline injection is performed. The patient has an IV in place in the antecubital region (between the arm and forearm, in the arm opposite the elbow). A small amount of air is mixed vigorously with saline to create numerous small bubbles and then this is injected through the patient’s IV. If a patient does not have a PFO, the bubbles will be visualized under ultrasound as entering the right atrium of the heart, but do not enter the left atrium because they have traveled to the lungs, which filter them. However, if a PFO is present, in many cases bubbles will be visualized entering the left atrium. Typically two injections are performed: one at rest, and one following the Valsalva maneuver, which involves bearing down/straining, as if lifting a heavy load or having a bowel movement. This maneuver increases return of blood to the right atrium, and a PFO that may not be significantly shunting blood to the left atrium at rest may suddenly enlarge when increased filling takes place in the right atrium, so the bubble test may be more dramatic.
There are limitations though. Breast tissue, obesity, and other factors may limit the viewing capabilities through the chest wall to detect bubbles in the left atrium. Sometimes, for no obvious reason, the study is just not of the quality needed to determine if a PFO is present. A transesophageal echocardiogram involves sedating a patient and inserting the ultrasound proble down the patient’s esophagus for a different view of the heart. This is thought to be a more sensitive study. The limitation to this test is that a sedated patient typically cannot be engaged in the procedure to voluntarily perform the Valsalva maneuver, so a PFO that is only a significant presence during such a maneuver may be missed.

This image compares three transcranial Doppler studies in patients with positive bubble studies for PFOs. The top image is from a patient with a PFO that is likely very small and which only allows a small degree of shunting from the right to left atrium. Each red vertical line represents a microbubble that has crossed to the left atrium and been detected in the brain during the test. The strip in the middle is from a patient with a moderate amount of shunting – more red lines/microemboli detected, but each one is still discernible from those around it. The bottom strip demonstrates the “shower effect.” The PFO is large and there is so much shunting that the microemboli are too numerous to count. Image source: http://www.revespcardiol.org
Transcranial Doppler is a study using ultrasound that measures blood flow within the major arteries of the brain. The same bubble study described above during an echocardiogram can be performed while blood flow is monitored in the middle cerebral arteries of the brain, and the detection of microemboli (small “blips” heard during monitoring) following the injection indicates that some form of passage from right-sided circulation to left-sided circulation is taking place. The limitation here is that pulmonary shunts, or vessels carrying blood directly from arterial to venous circulation within a lung, can also give a positive bubble test since transcranial Doppler does not involve the direct visualization of bubbles. However, signals are detected later than expected if the shunting is occurring in the lungs (more cardiac cycles following the injection than the timing of when signals from bubbles crossing through a PFO would be heard).
Transcranial Doppler is sensitive in detecting a PFO, and if consistent with this should be followed up with an echocardiogram, if not already performed.
If a PFO is detected, what then? This can be a challenging question to answer, in part because it is impossible to prove whether the PFO actually played a role in the stroke, or if another factor was at play and the PFO is just receiving the blame unnecessarily.
The question of whether to continue a stroke patient with a PFO and without another obvious cause of stroke on medical therapy or to close the PFO has been tested in at least two randomized clinical trials – CLOSURE I and RESPECT.
The CLOSURE I trial failed to show a significant benefit to PFO closure over medical therapy. However, CLOSURE I enrolled patients with either evidence of stroke on brain imaging or patients with “TIA.” The reason I place the term TIA in quotes is because more than half of the consults I see for diagnosis of “TIA” do not turn out to be actual TIAs, but migraines, seizures, or other conditions that mimick TIAs. The point here is that many neurologists argued that the validity of CLOSURE I results was negatively impacted by potentially enrolling patients into the trial with PFOs who had not actually had a vascular event, and that this may have skewed the data.
The RESPECT trial randomized young patients with PFOs and who sustained strokes without a known origin to either receive “best medical therapy” or to undergo PFO closure in addition to remaining on “best medical therapy.” There was no significant difference in stroke outcomes between the two groups, but may have been some benefit in patients with large PFOs or with aneurysmal atrial septum.
RESPECT was a trial randomizing only relatively young stroke patients with PFOs (no TIAs were included – there had to be evidence of stroke on the patient’s neuroimaging) who lacked another apparent source for the stroke to either PFO closure plus medical therapy, or medical therapy alone for stroke prevention. The overall trial failed to show benefit to PFO closure over medical therapy alone. However, in a secondary analysis, patients who had large PFOs or who had a finding known as an atrial septal aneurysm (very mobile wall separating the two halves of the heart) did show more potential benefit for stroke prevention from PFO closure and medical therapy than from medical therapy alone.
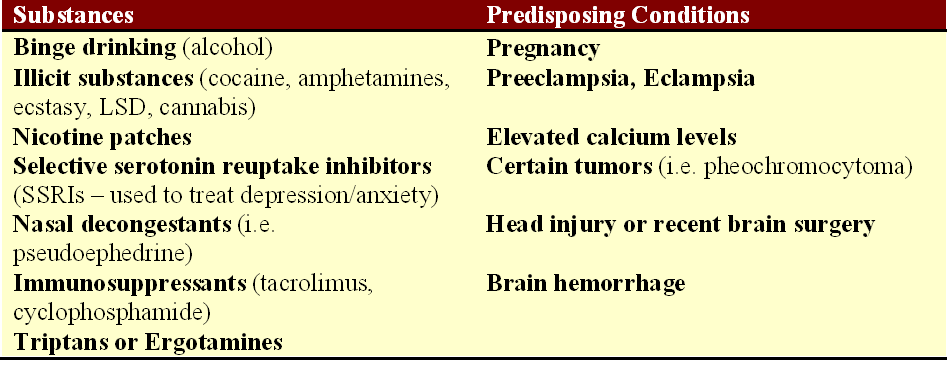
What is medical therapy? Medical therapy refers to any non-invasive therapy measures taken, in this case – to reduce the risk of another stroke. For patients with small PFOs and no history of stroke, this usually meant aspirin daily. For patients with atrial septal aneurysm, there is some data suggesting a relatively high risk of stroke recurrence on aspirin, but that anticoagulation may be more beneficial. I have found that the type of “best medical therapy” recommended to a patient often plays a role in his or her decision regarding PFO closure. Patients are often more willing to take aspirin daily over undergoing PFO closure, but many young patients are not thrilled with the idea of anticoagulation and the risks it carries over the long term.
It is mostly performed now via catheterization with an implanted device sealing the opening between the right and left atria. The procedure typically lasts less than one hour from start to finish, and patients usually go home from the hospital the following day. At some hospitals, they may even return home on the same day. There are potential complications to a PFO closure, including bleeding, infection, and the potential for atrial fibrillation, an irregular cardiac rhythm that can generate clots and result in stroke. Based on data from RESPECT, the incidence of atrial fibrillation did not differ significantly between the PFO closure group and the medical therapy alone group.
Following the publication of RESPECT trial results, PFO closure remains a topic of controversy in the field of stroke prevention and is still heavily debated.